 Those of you who have previously read my blog know that I rarely use children’s games to address language goals. However, over the summer I have been working on improving executive function abilities (EFs) of some of the language impaired students on my caseload. As such, I found select children’s games to be highly beneficial for improving language-based executive function abilities.
Those of you who have previously read my blog know that I rarely use children’s games to address language goals. However, over the summer I have been working on improving executive function abilities (EFs) of some of the language impaired students on my caseload. As such, I found select children’s games to be highly beneficial for improving language-based executive function abilities.
For those of you who are only vaguely familiar with this concept, executive functions are higher level cognitive processes involved in the inhibition of thought, action, and emotion, which located in the prefrontal cortex of the frontal lobe of the brain. The development of executive functions begins in early infancy; but it can be easily disrupted by a number of adverse environmental and organic experiences (e.g., psychosocial deprivation, trauma). Furthermore, research in this area indicates that the children with language impairments present with executive function weaknesses which require remediation.
EF components include working memory, inhibitory control, planning, and set-shifting.
- Working memory
- Ability to store and manipulate information in mind over brief periods of time
- Inhibitory control
- Suppressing responses that are not relevant to the task
- Set-shifting
- Ability to shift behavior in response to changes in tasks or environment
Simply put, EFs contribute to the child’s ability to sustain attention, ignore distractions, and succeed in academic settings. By now some of you must be wondering: “So what does Hedbanz have to do with any of it?”
Well, Hedbanz is a quick-paced multiplayer (2-6 people) game of “What Am I?” for children ages 7 and up. Players get 3 chips and wear a “picture card” in their headband. They need to ask questions in rapid succession to figure out what they are. “Am I fruit?” “Am I a dessert?” “Am I sports equipment?” When they figure it out, they get rid of a chip. The first player to get rid of all three chips wins.
The game sounds deceptively simple. Yet if any SLPs or parents have ever played that game with their language impaired students/children as they would be quick to note how extraordinarily difficult it is for the children to figure out what their card is. Interestingly, in my clinical experience, I’ve noticed that it’s not just moderately language impaired children who present with difficulty playing this game. Even my bright, average intelligence teens, who have passed vocabulary and semantic flexibility testing (such as the WORD Test 2-Adolescent or the Vocabulary Awareness subtest of the Test of Integrated Language and Literacy ) significantly struggle with their language organization when playing this game.
So what makes Hedbanz so challenging for language impaired students? Primarily, it’s the involvement and coordination of the multiple executive functions during the game. In order to play Hedbanz effectively and effortlessly, the following EF involvement is needed:
- Task Initiation
- Students with executive function impairments will often “freeze up” and as a result may have difficulty initiating the asking of questions in the game because many will not know what kind of questions to ask, even after extensive explanations and elaborations by the therapist.
- Organization
- Students with executive function impairments will present with difficulty organizing their questions by meaningful categories and as a result will frequently lose their track of thought in the game.
- Working Memory
- This executive function requires the student to keep key information in mind as well as keep track of whatever questions they have already asked.
- Flexible Thinking
- This executive function requires the student to consider a situation from multiple angles in order to figure out the quickest and most effective way of arriving at a solution. During the game, students may present with difficulty flexibly generating enough organizational categories in order to be effective participants.
- Impulse Control
- Many students with difficulties in this area may blurt out an inappropriate category or in an appropriate question without thinking it through first.
- They may also present with difficulty set-shifting. To illustrate, one of my 13-year-old students with ASD, kept repeating the same question when it was his turn, despite the fact that he was informed by myself as well as other players of the answer previously.
- Many students with difficulties in this area may blurt out an inappropriate category or in an appropriate question without thinking it through first.
- Emotional Control
- This executive function will help students with keeping their emotions in check when the game becomes too frustrating. Many students of difficulties in this area will begin reacting behaviorally when things don’t go their way and they are unable to figure out what their card is quickly enough. As a result, they may have difficulty mentally regrouping and reorganizing their questions when something goes wrong in the game.
- Self-Monitoring
- This executive function allows the students to figure out how well or how poorly they are doing in the game. Students with poor insight into own abilities may present with difficulty understanding that they are doing poorly and may require explicit instruction in order to change their question types.
- Planning and Prioritizing
- Students with poor abilities in this area will present with difficulty prioritizing their questions during the game.
Consequently, all of the above executive functions can be addressed via language-based goals. However, before I cover that, I’d like to review some of my session procedures first.
Typically, long before game initiation, I use the cards from the game to prep the students by teaching them how to categorize and classify presented information so they effectively and efficiently play the game.
 Rather than using the “tip cards”, I explain to the students how to categorize information effectively.
Rather than using the “tip cards”, I explain to the students how to categorize information effectively.
This, in turn, becomes a great opportunity for teaching students relevant vocabulary words, which can be extended far beyond playing the game.
I begin the session by explaining to the students that pretty much everything can be roughly divided into two categories animate (living) or inanimate (nonliving) things. I explain that humans, animals, as well as plants belong to the category of living things, while everything else belongs to the category of inanimate objects. I further divide the category of inanimate things into naturally existing and man-made items. I explain to the students that the naturally existing category includes bodies of water, landmarks, as well as things in space (moon, stars, sky, sun, etc.). In contrast, things constructed in factories or made by people would be example of man-made objects (e.g., building, aircraft, etc.)
When I’m confident that the students understand my general explanations, we move on to discuss further refinement of these broad categories. If a student determines that their card belongs to the category of living things, we discuss how from there the student can further determine whether they are an animal, a plant, or a human. If a student determined that their card belongs to the animal category, we discuss how we can narrow down the options of figuring out what animal is depicted on their card by asking questions regarding their habitat (“Am I a jungle animal?”), and classification (“Am I a reptile?”). From there, discussion of attributes prominently comes into play. We discuss shapes, sizes, colors, accessories, etc., until the student is able to confidently figure out which animal is depicted on their card.
In contrast, if the student’s card belongs to the inanimate category of man-made objects, we further subcategorize the information by the object’s location (“Am I found outside or inside?”; “Am I found in ___ room of the house?”, etc.), utility (“Can I be used for ___?”), as well as attributes (e.g., size, shape, color, etc.)
Thus, in addition to improving the students’ semantic flexibility skills (production of definitions, synonyms, attributes, etc.) the game teaches the students to organize and compartmentalize information in order to effectively and efficiently arrive at a conclusion in the most time expedient fashion.
Now, we are ready to discuss what type of EF language-based goals, SLPs can target by simply playing this game.
1. Initiation: Student will initiate questioning during an activity in __ number of instances per 30-minute session given (maximal, moderate, minimal) type of ___ (phonemic, semantic, etc.) prompts and __ (visual, gestural, tactile, etc.) cues by the clinician.
2. Planning: Given a specific routine, student will verbally state the order of steps needed to complete it with __% accuracy given (maximal, moderate, minimal) type of ___ (phonemic, semantic, etc.) prompts and __ (visual, gestural, tactile, etc.) cues by the clinician.
3. Working Memory: Student will repeat clinician provided verbal instructions pertaining to the presented activity, prior to its initiation, with 80% accuracy given (maximal, moderate, minimal) type of ___ (phonemic, semantic, etc.) prompts and __ (visual, gestural, tactile, etc.) cues by the clinician.
4. Flexible Thinking: Following a training by the clinician, student will generate at least __ questions needed for task completion (e.g., winning the game) with __% accuracy given (maximal, moderate, minimal) type of ___ (phonemic, semantic, etc.) prompts and __ (visual, gestural, tactile, etc.) cues by the clinician.
5. Organization: Student will use predetermined written/visual cues during an activity to assist self with organization of information (e.g., questions to ask) with __% accuracy given (maximal, moderate, minimal) type of ___ (phonemic, semantic, etc.) prompts and __ (visual, gestural, tactile, etc.) cues by the clinician.
6. Impulse Control: During the presented activity the student will curb blurting out inappropriate responses (by silently counting to 3 prior to providing his response) in __ number of instances per 30 minute session given (maximal, moderate, minimal) type of ___ (phonemic, semantic, etc.) prompts and __ (visual, gestural, tactile, etc.) cues by the clinician.
7. Emotional Control: When upset, student will verbalize his/her frustration (vs. behavioral activing out) in __ number of instances per 30 minute session given (maximal, moderate, minimal) type of ___ (phonemic, semantic, etc.) prompts and __ (visual, gestural, tactile, etc.) cues by the clinician.
8. Self-Monitoring: Following the completion of an activity (e.g., game) student will provide insight into own strengths and weaknesses during the activity (recap) by verbally naming the instances in which s/he did well, and instances in which s/he struggled with __% accuracy given (maximal, moderate, minimal) type of ___ (phonemic, semantic, etc.) prompts and __ (visual, gestural, tactile, etc.) cues by the clinician.
There you have it. This one simple game doesn’t just target a plethora of typical expressive language goals. It can effectively target and improve language-based executive function goals as well. Considering the fact that it sells for approximately $12 on Amazon.com, that’s a pretty useful therapy material to have in one’s clinical tool repertoire. For fancier versions, clinicians can use “Jeepers Peepers” photo card sets sold by Super Duper Inc. Strapped for cash, due to highly limited budget? You can find plenty of free materials online if you simply input “Hedbanz cards” in your search query on Google. So have a little fun in therapy, while your students learn something valuable in the process and play Hedbanz today!
Related Smart Speech Therapy Resources:

 Assessment of motor speech disorders in young children requires solid knowledge and expertise. That is because CAS has a number of overlapping symptoms with other speech sound disorders (e.g., severe phonological disorder, dysarthria, etc). Furthermore, symptoms which may initially appear as CAS may change during the course of intervention by the time the child is older (e.g., 3 years of age) which is why diagnosing toddlers under 3 years of age is very problematic and the use of “suspected” or “working” diagnosis is recommended (Davis & Velleman, 2000) in order to avoid misdiagnosis. Finally, the diagnosis of CAS is also problematic due to the fact that there are still to this day no valid or reliable standardized assessments sensitive to CAS detection (McCauley & Strand, 2008).
Assessment of motor speech disorders in young children requires solid knowledge and expertise. That is because CAS has a number of overlapping symptoms with other speech sound disorders (e.g., severe phonological disorder, dysarthria, etc). Furthermore, symptoms which may initially appear as CAS may change during the course of intervention by the time the child is older (e.g., 3 years of age) which is why diagnosing toddlers under 3 years of age is very problematic and the use of “suspected” or “working” diagnosis is recommended (Davis & Velleman, 2000) in order to avoid misdiagnosis. Finally, the diagnosis of CAS is also problematic due to the fact that there are still to this day no valid or reliable standardized assessments sensitive to CAS detection (McCauley & Strand, 2008). Prior to being reevaluated by me, TQ underwent an early intervention assessment at ~26 months of age. She was diagnosed with CAS by an evaluating SLP and was found to be eligible for speech-language services, which she began receiving shortly thereafter. However, Mrs. Q noted that TQ was making very few gains in therapy and her treating SLP was uncertain regarding why her progress in therapy was so limited. Mrs. Q was also rather uncertain that TQ’s diagnosis of CAS was indeed a correct one, which was another reason why she sought a second opinion.
Prior to being reevaluated by me, TQ underwent an early intervention assessment at ~26 months of age. She was diagnosed with CAS by an evaluating SLP and was found to be eligible for speech-language services, which she began receiving shortly thereafter. However, Mrs. Q noted that TQ was making very few gains in therapy and her treating SLP was uncertain regarding why her progress in therapy was so limited. Mrs. Q was also rather uncertain that TQ’s diagnosis of CAS was indeed a correct one, which was another reason why she sought a second opinion. TQ’s oral peripheral examination yielded no difficulties with oral movements during non-speaking as well as speaking tasks. She was able to blow bubbles, stick out tongue, smile, etc as well as spontaneously vocalize without any difficulties. Her voice quality, pitch, loudness, and resonance during vocalizations and approximated utterances were judged to be appropriate for age and gender. Her prosody and fluency could not be determined due to lack of spontaneously produced continuous verbal output.
TQ’s oral peripheral examination yielded no difficulties with oral movements during non-speaking as well as speaking tasks. She was able to blow bubbles, stick out tongue, smile, etc as well as spontaneously vocalize without any difficulties. Her voice quality, pitch, loudness, and resonance during vocalizations and approximated utterances were judged to be appropriate for age and gender. Her prosody and fluency could not be determined due to lack of spontaneously produced continuous verbal output. I felt that the diagnosis of CAS was not applicable because TQ lacked a verbal lexicon and no specific phonological intervention techniques had been trialed with her during the course of her brief therapy (~4 months) to elicit word productions (Davis & Velleman, 2000; Strand, 2003). While her EI speech therapist documented that therapy has primarily focused on ‘oral motor activities to increase TQ’s awareness of her articulators and to increase imitation of oral motor movements’, I knew that until a variety of phonological/motor-speech specific interventions had been trialed over a period of time (at least ~6 months as per Davis & Velleman, 2000) the diagnosis of CAS could not be reliably made.
I felt that the diagnosis of CAS was not applicable because TQ lacked a verbal lexicon and no specific phonological intervention techniques had been trialed with her during the course of her brief therapy (~4 months) to elicit word productions (Davis & Velleman, 2000; Strand, 2003). While her EI speech therapist documented that therapy has primarily focused on ‘oral motor activities to increase TQ’s awareness of her articulators and to increase imitation of oral motor movements’, I knew that until a variety of phonological/motor-speech specific interventions had been trialed over a period of time (at least ~6 months as per Davis & Velleman, 2000) the diagnosis of CAS could not be reliably made. *For those of you who are interested in the latest EBP treatment for motor speech disorders, current evidence supports the use of the
*For those of you who are interested in the latest EBP treatment for motor speech disorders, current evidence supports the use of the  Now I know that some clinicians will be quick to ask me: “What’s the harm in overdiagnosing CAS if the child’s speech production will still be treated via the application of motor speech production principles?” Well, aside from the fact that it’s obviously unethical and can result in terrifying the parents into obtaining all sorts of
Now I know that some clinicians will be quick to ask me: “What’s the harm in overdiagnosing CAS if the child’s speech production will still be treated via the application of motor speech production principles?” Well, aside from the fact that it’s obviously unethical and can result in terrifying the parents into obtaining all sorts of  Today, I’d like to talk about speech and language assessments of children under three years of age. Namely, the quality of these assessments. Let me be frank, I am not happy with what I am seeing. Often times, when I receive a speech-language report on a child under three years of age, I am struck by how little functional information it contains about the child’s linguistic strengths and weaknesses. Indeed, conversations with parents often reveal that at best the examiner spent no more than half an hour or so playing with the child and performed very limited functional testing of their actual abilities. Instead, they interviewed the parent and based their report on parental feedback alone. Consequently, parents often end up with a report of very limited value, which does not contain any helpful information on how delayed is the child as compared to peers their age.
Today, I’d like to talk about speech and language assessments of children under three years of age. Namely, the quality of these assessments. Let me be frank, I am not happy with what I am seeing. Often times, when I receive a speech-language report on a child under three years of age, I am struck by how little functional information it contains about the child’s linguistic strengths and weaknesses. Indeed, conversations with parents often reveal that at best the examiner spent no more than half an hour or so playing with the child and performed very limited functional testing of their actual abilities. Instead, they interviewed the parent and based their report on parental feedback alone. Consequently, parents often end up with a report of very limited value, which does not contain any helpful information on how delayed is the child as compared to peers their age. Why 30 months, you may ask? Well, there isn’t really any hard science to it. It’s just that I noticed that a significant percentage of parents who were already worried about their children’s speech-language abilities when they were younger, begin to act upon those worries as the child is nearing 3 years of age and their abilities are not improving or are not commensurate with other peers their age.
Why 30 months, you may ask? Well, there isn’t really any hard science to it. It’s just that I noticed that a significant percentage of parents who were already worried about their children’s speech-language abilities when they were younger, begin to act upon those worries as the child is nearing 3 years of age and their abilities are not improving or are not commensurate with other peers their age. At this point, I am ready to move on to the language portion of the assessment. Here it is important to note that a number of assessments for toddlers under 3 years of age contain numerous limitations. Some such as REEL-3 or Rosetti (a criterion-referenced vs. normed-referenced instrument) are observational or limitedly interactive in nature, while others such as PLS-5, have a tendency to
At this point, I am ready to move on to the language portion of the assessment. Here it is important to note that a number of assessments for toddlers under 3 years of age contain numerous limitations. Some such as REEL-3 or Rosetti (a criterion-referenced vs. normed-referenced instrument) are observational or limitedly interactive in nature, while others such as PLS-5, have a tendency to  Now I know that many of you will tell me, that this is a ‘perfect world’ evaluation conducted by a private therapist with an unlimited amount of time on her hands. And to some extent, many of you will be right! Yes, such an evaluation was a result of more than 30 minutes spent face-to-face with the child. All in all, it took probably closer to 90 minutes of face to face time to complete it and a few hours to write. And yes, this is a luxury only a few possess and many therapists in the early intervention system lack. But in the long run, such evaluations pay dividends not only, obviously, to your clients but to SLPs who perform them. They enhance and grow your reputation as an evaluating therapist. They even make sense from a business perspective. If you are well-known and highly sought after due to your evaluating expertise, you can expect to be compensated for your time, accordingly. This means that if you decide that your time and expertise are worth private pay only (due to poor insurance reimbursement or low EI rates), you can be sure that parents will learn to appreciate your thoroughness and will choose you over other providers.
Now I know that many of you will tell me, that this is a ‘perfect world’ evaluation conducted by a private therapist with an unlimited amount of time on her hands. And to some extent, many of you will be right! Yes, such an evaluation was a result of more than 30 minutes spent face-to-face with the child. All in all, it took probably closer to 90 minutes of face to face time to complete it and a few hours to write. And yes, this is a luxury only a few possess and many therapists in the early intervention system lack. But in the long run, such evaluations pay dividends not only, obviously, to your clients but to SLPs who perform them. They enhance and grow your reputation as an evaluating therapist. They even make sense from a business perspective. If you are well-known and highly sought after due to your evaluating expertise, you can expect to be compensated for your time, accordingly. This means that if you decide that your time and expertise are worth private pay only (due to poor insurance reimbursement or low EI rates), you can be sure that parents will learn to appreciate your thoroughness and will choose you over other providers. In recent years there has been an increase in research on the subject of diagnosis and treatment of Auditory Processing Disorders (APD), formerly known as Central Auditory Processing Disorders or CAPD.
In recent years there has been an increase in research on the subject of diagnosis and treatment of Auditory Processing Disorders (APD), formerly known as Central Auditory Processing Disorders or CAPD. Today it is my pleasure and privilege to interview 3 Australian lactation consultations: Lois Wattis, Renee Kam, and Pamela Douglas, the authors of a March 2017 article in the Breastfeeding Review: “Three experienced lactation consultants reflect upon the oral tie phenomenon” (which can be found
Today it is my pleasure and privilege to interview 3 Australian lactation consultations: Lois Wattis, Renee Kam, and Pamela Douglas, the authors of a March 2017 article in the Breastfeeding Review: “Three experienced lactation consultants reflect upon the oral tie phenomenon” (which can be found  Presently, systematic reviews1-3 demonstrate there is insufficient evidence for the above. However, when many professionals including myself, cite reputable research explaining the lack of support of surgical intervention for tongue tie, there has been a pushback on the part of a number of other health professionals including lactation consultants, nurses, dentists, as well as speech-language pathologists stating that in their clinical experience surgical intervention does resolve issues with tongue tie as related to speech and feeding.
Presently, systematic reviews1-3 demonstrate there is insufficient evidence for the above. However, when many professionals including myself, cite reputable research explaining the lack of support of surgical intervention for tongue tie, there has been a pushback on the part of a number of other health professionals including lactation consultants, nurses, dentists, as well as speech-language pathologists stating that in their clinical experience surgical intervention does resolve issues with tongue tie as related to speech and feeding.
 Pamela Douglas:
Pamela Douglas: 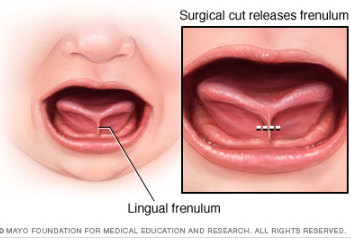
 Tatyana Elleseff: Thank you! This is highly relevant information for both health professionals and parents alike. I truly appreciate your clinical expertise on this topic. While we are on the topic of restrictive lingual frenulums can we discuss several recent articles published on surgical interventions for the above? For example (Ghaheri, Cole, Fausel, Chuop & Mace, 2016), recently published the result of their study which concluded that: “Surgical release of tongue-tie/lip-tie results in significant improvement in breastfeeding outcomes”. Can you elucidate upon the study design and its findings?
Tatyana Elleseff: Thank you! This is highly relevant information for both health professionals and parents alike. I truly appreciate your clinical expertise on this topic. While we are on the topic of restrictive lingual frenulums can we discuss several recent articles published on surgical interventions for the above? For example (Ghaheri, Cole, Fausel, Chuop & Mace, 2016), recently published the result of their study which concluded that: “Surgical release of tongue-tie/lip-tie results in significant improvement in breastfeeding outcomes”. Can you elucidate upon the study design and its findings? Tatyana Elleseff: Thank you for that. In addition to studies on tongue tie revisions and breastfeeding outcomes, there has been an increase in studies, specifically Kotlow (2016) and Siegel (2016), which claimed that surgical intervention improves outcomes for acid reflux and aerophagia in babies”. Can you discuss these studies design and findings?
Tatyana Elleseff: Thank you for that. In addition to studies on tongue tie revisions and breastfeeding outcomes, there has been an increase in studies, specifically Kotlow (2016) and Siegel (2016), which claimed that surgical intervention improves outcomes for acid reflux and aerophagia in babies”. Can you discuss these studies design and findings? There you have it, readers. Both research and clinical practice align to indicate that:
There you have it, readers. Both research and clinical practice align to indicate that: Since many children with restricted frenulum do not have any speech production difficulties, Dr Kummer explains why that is the case by discussing
Since many children with restricted frenulum do not have any speech production difficulties, Dr Kummer explains why that is the case by discussing 



 For bilingual and monolingual SLPs working with bilingual and multicultural children, the question of: “Is it a difference or a disorder?” arises on a daily basis as they attempt to navigate the myriad of difficulties they encounter in their attempts at appropriate diagnosis of speech, language, and literacy disorders.
For bilingual and monolingual SLPs working with bilingual and multicultural children, the question of: “Is it a difference or a disorder?” arises on a daily basis as they attempt to navigate the myriad of difficulties they encounter in their attempts at appropriate diagnosis of speech, language, and literacy disorders. For that purpose, I’ve recently created a
For that purpose, I’ve recently created a 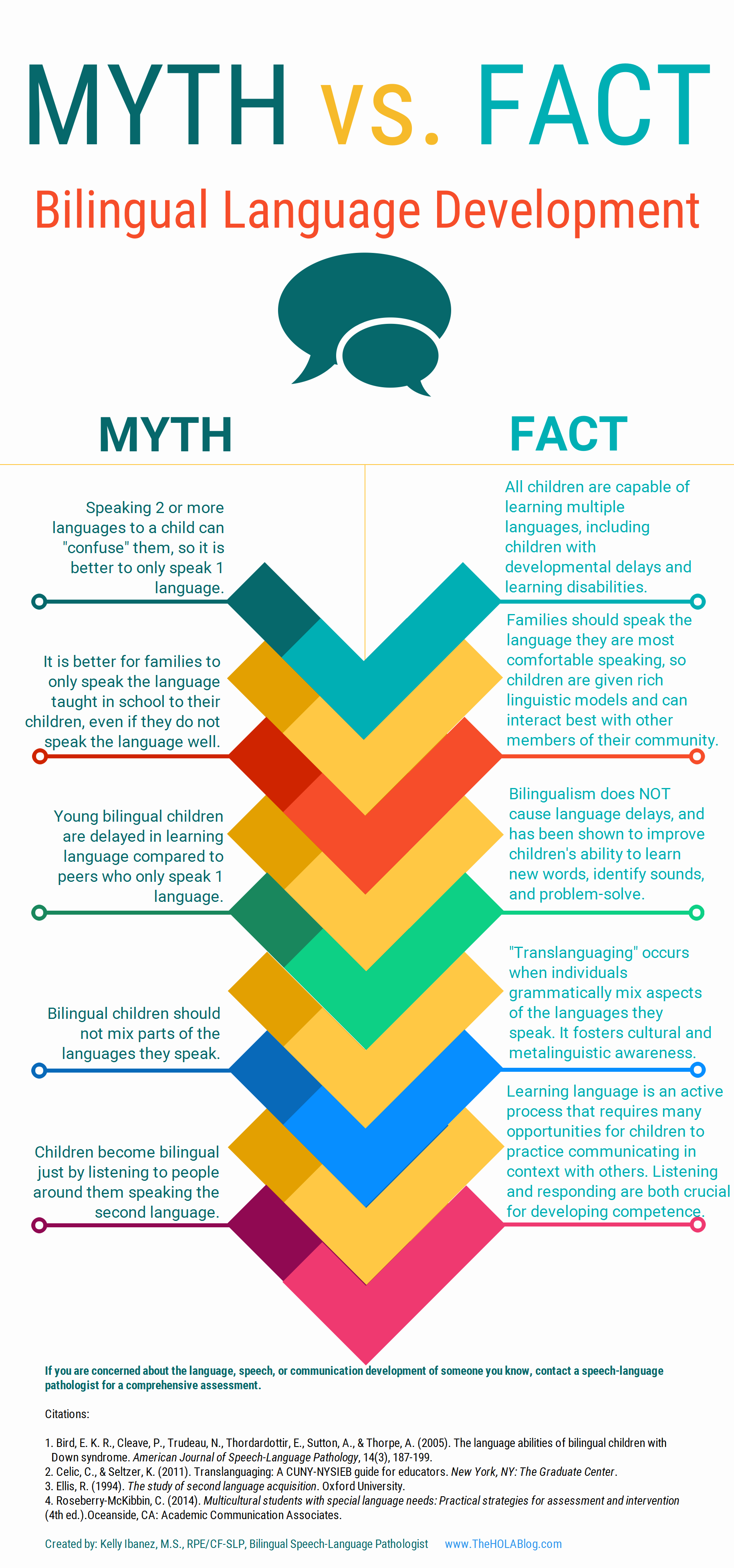 Let’s start with an excellent free infographic entitled from the Hola Blog “
Let’s start with an excellent free infographic entitled from the Hola Blog “ Next up, is a great archive which contains
Next up, is a great archive which contains  For SLPs working with Russian-speaking children the following links pertinent to assessment, intervention and language transference may be helpful:
For SLPs working with Russian-speaking children the following links pertinent to assessment, intervention and language transference may be helpful: In recent months, I have been focusing more and more on speaking engagements as well as the development of products with an explicit focus on assessment and intervention of literacy in speech-language pathology. Today I’d like to introduce 4 of my recently developed products pertinent to assessment and treatment of literacy in speech-language pathology.
In recent months, I have been focusing more and more on speaking engagements as well as the development of products with an explicit focus on assessment and intervention of literacy in speech-language pathology. Today I’d like to introduce 4 of my recently developed products pertinent to assessment and treatment of literacy in speech-language pathology. First up is the
First up is the  Next up is a product entitled
Next up is a product entitled  The product
The product  Finally, my last product
Finally, my last product 

 High comorbidity between language and psychiatric disorders has been well documented (Beitchman, Cohen, Konstantaras, & Tannock, 1996; Cohen, Barwick, Horodezky, Vallence, & Im, 1998; Toppelberg & Shapiro, 2000). However, a lesser known fact is that there’s also a significant under-diagnosis of language impairments in children with psychiatric disorders.
High comorbidity between language and psychiatric disorders has been well documented (Beitchman, Cohen, Konstantaras, & Tannock, 1996; Cohen, Barwick, Horodezky, Vallence, & Im, 1998; Toppelberg & Shapiro, 2000). However, a lesser known fact is that there’s also a significant under-diagnosis of language impairments in children with psychiatric disorders. 
