 The Test of Integrated Language & Literacy Skills (TILLS) is an assessment of oral and written language abilities in students 6–18 years of age. Published in the Fall 2015, it is unique in the way that it is aimed to thoroughly assess skills such as reading fluency, reading comprehension, phonological awareness, spelling, as well as writing in school age children. As I have been using this test since the time it was published, I wanted to take an opportunity today to share just a few of my impressions of this assessment.
The Test of Integrated Language & Literacy Skills (TILLS) is an assessment of oral and written language abilities in students 6–18 years of age. Published in the Fall 2015, it is unique in the way that it is aimed to thoroughly assess skills such as reading fluency, reading comprehension, phonological awareness, spelling, as well as writing in school age children. As I have been using this test since the time it was published, I wanted to take an opportunity today to share just a few of my impressions of this assessment.


First, a little background on why I chose to purchase this test so shortly after I had purchased the Clinical Evaluation of Language Fundamentals – 5 (CELF-5). Soon after I started using the CELF-5 I noticed that it tended to considerably overinflate my students’ scores on a variety of its subtests. In fact, I noticed that unless a student had a fairly severe degree of impairment, the majority of his/her scores came out either low/slightly below average (click for more info on why this was happening HERE, HERE, or HERE). Consequently, I was excited to hear regarding TILLS development, almost simultaneously through ASHA as well as SPELL-Links ListServe. I was particularly happy because I knew some of this test’s developers (e.g., Dr. Elena Plante, Dr. Nickola Nelson) have published solid research in the areas of psychometrics and literacy respectively.

According to the TILLS developers it has been standardized for 3 purposes:
- to identify language and literacy disorders
- to document patterns of relative strengths and weaknesses
- to track changes in language and literacy skills over time
The testing subtests can be administered in isolation (with the exception of a few) or in its entirety. The administration of all the 15 subtests may take approximately an hour and a half, while the administration of the core subtests typically takes ~45 mins).
Please note that there are 5 subtests that should not be administered to students 6;0-6;5 years of age because many typically developing students are still mastering the required skills.
- Subtest 5 – Nonword Spelling
- Subtest 7 – Reading Comprehension
- Subtest 10 – Nonword Reading
- Subtest 11 – Reading Fluency
- Subtest 12 – Written Expression
However, if needed, there are several tests of early reading and writing abilities which are available for assessment of children under 6:5 years of age with suspected literacy deficits (e.g., TERA-3: Test of Early Reading Ability–Third Edition; Test of Early Written Language, Third Edition-TEWL-3, etc.).
Let’s move on to take a deeper look at its subtests. Please note that for the purposes of this review all images came directly from and are the property of Brookes Publishing Co (clicking on each of the below images will take you directly to their source).
 1. Vocabulary Awareness (VA) (description above) requires students to display considerable linguistic and cognitive flexibility in order to earn an average score. It works great in teasing out students with weak vocabulary knowledge and use, as well as students who are unable to quickly and effectively analyze words for deeper meaning and come up with effective definitions of all possible word associations. Be mindful of the fact that even though the words are presented to the students in written format in the stimulus book, the examiner is still expected to read all the words to the students. Consequently, students with good vocabulary knowledge and strong oral language abilities can still pass this subtest despite the presence of significant reading weaknesses. Recommendation: I suggest informally checking the student’s word reading abilities by asking them to read of all the words, before reading all the word choices to them. This way you can informally document any word misreadings made by the student even in the presence of an average subtest score.
1. Vocabulary Awareness (VA) (description above) requires students to display considerable linguistic and cognitive flexibility in order to earn an average score. It works great in teasing out students with weak vocabulary knowledge and use, as well as students who are unable to quickly and effectively analyze words for deeper meaning and come up with effective definitions of all possible word associations. Be mindful of the fact that even though the words are presented to the students in written format in the stimulus book, the examiner is still expected to read all the words to the students. Consequently, students with good vocabulary knowledge and strong oral language abilities can still pass this subtest despite the presence of significant reading weaknesses. Recommendation: I suggest informally checking the student’s word reading abilities by asking them to read of all the words, before reading all the word choices to them. This way you can informally document any word misreadings made by the student even in the presence of an average subtest score.
2. The Phonemic Awareness (PA) subtest (description above) requires students to isolate and delete initial sounds in words of increasing complexity. While this subtest does not require sound isolation and deletion in various word positions, similar to tests such as the CTOPP-2: Comprehensive Test of Phonological Processing–Second Edition or the The Phonological Awareness Test 2 (PAT 2), it is still a highly useful and reliable measure of phonemic awareness (as one of many precursors to reading fluency success). This is especially because after the initial directions are given, the student is expected to remember to isolate the initial sounds in words without any prompting from the examiner. Thus, this task also indirectly tests the students’ executive function abilities in addition to their phonemic awareness skills.
3. The Story Retelling (SR) subtest (description above) requires students to do just that retell a story. Be mindful of the fact that the presented stories have reduced complexity. Thus, unless the students possess significant retelling deficits, the above subtest may not capture their true retelling abilities. Recommendation: Consider supplementing this subtest with informal narrative measures. For younger children (kindergarten and first grade) I recommend using wordless picture books to perform a dynamic assessment of their retelling abilities following a clinician’s narrative model (e.g., HERE). For early elementary aged children (grades 2 and up), I recommend using picture books, which are first read to and then retold by the students with the benefit of pictorial but not written support. Finally, for upper elementary aged children (grades 4 and up), it may be helpful for the students to retell a book or a movie seen recently (or liked significantly) by them without the benefit of visual support all together (e.g., HERE).

4. The Nonword Repetition (NR) subtest (description above) requires students to repeat nonsense words of increasing length and complexity. Weaknesses in the area of nonword repetition have consistently been associated with language impairments and learning disabilities due to the task’s heavy reliance on phonological segmentation as well as phonological and lexical knowledge (Leclercq, Maillart, Majerus, 2013). Thus, both monolingual and simultaneously bilingual children with language and literacy impairments will be observed to present with patterns of segment substitutions (subtle substitutions of sounds and syllables in presented nonsense words) as well as segment deletions of nonword sequences more than 2-3 or 3-4 syllables in length (depending on the child’s age).
5. The Nonword Spelling (NS) subtest (description above) requires the students to spell nonwords from the Nonword Repetition (NR) subtest. Consequently, the Nonword Repetition (NR) subtest needs to be administered prior to the administration of this subtest in the same assessment session. In contrast to the real-word spelling tasks, students cannot memorize the spelling of the presented words, which are still bound by orthographic and phonotactic constraints of the English language. While this is a highly useful subtest, is important to note that simultaneously bilingual children may present with decreased scores due to vowel errors. Consequently, it is important to analyze subtest results in order to determine whether dialectal differences rather than a presence of an actual disorder is responsible for the error patterns.
6. The Listening Comprehension (LC) subtest (description above) requires the students to listen to short stories and then definitively answer story questions via available answer choices, which include: “Yes”, “No’, and “Maybe”. This subtest also indirectly measures the students’ metalinguistic awareness skills as they are needed to detect when the text does not provide sufficient information to answer a particular question definitively (e.g., “Maybe” response may be called for). Be mindful of the fact that because the students are not expected to provide sentential responses to questions it may be important to supplement subtest administration with another listening comprehension assessment. Tests such as the Listening Comprehension Test-2 (LCT-2), the Listening Comprehension Test-Adolescent (LCT-A), or the Executive Function Test-Elementary (EFT-E) may be useful if language processing and listening comprehension deficits are suspected or reported by parents or teachers. This is particularly important to do with students who may be ‘good guessers’ but who are also reported to present with word-finding difficulties at sentence and discourse levels.
7. The Reading Comprehension (RC) subtest (description above) requires the students to read short story and answer story questions in “Yes”, “No’, and “Maybe” format. This subtest is not stand alone and must be administered immediately following the administration the Listening Comprehension subtest. The student is asked to read the first story out loud in order to determine whether s/he can proceed with taking this subtest or discontinue due to being an emergent reader. The criterion for administration of the subtest is making 7 errors during the reading of the first story and its accompanying questions. Unfortunately, in my clinical experience this subtest is not always accurate at identifying children with reading-based deficits.
While I find it terrific for students with severe-profound reading deficits and/or below average IQ, a number of my students with average IQ and moderately impaired reading skills managed to pass it via a combination of guessing and luck despite being observed to misread aloud between 40-60% of the presented words. Be mindful of the fact that typically such students may have up to 5-6 errors during the reading of the first story. Thus, according to administration guidelines these students will be allowed to proceed and take this subtest. They will then continue to make text misreadings during each story presentation (you will know that by asking them to read each story aloud vs. silently). However, because the response mode is in definitive (“Yes”, “No’, and “Maybe”) vs. open ended question format, a number of these students will earn average scores by being successful guessers. Recommendation: I highly recommend supplementing the administration of this subtest with grade level (or below grade level) texts (see HERE and/or HERE), to assess the student’s reading comprehension informally.
I present a full one page text to the students and ask them to read it to me in its entirety. I audio/video record the student’s reading for further analysis (see Reading Fluency section below). After the completion of the story I ask the student questions with a focus on main idea comprehension and vocabulary definitions. I also ask questions pertaining to story details. Depending on the student’s age I may ask them abstract/ factual text questions with and without text access. Overall, I find that informal administration of grade level (or even below grade-level) texts coupled with the administration of standardized reading tests provides me with a significantly better understanding of the student’s reading comprehension abilities rather than administration of standardized reading tests alone.
8. The Following Directions (FD) subtest (description above) measures the student’s ability to execute directions of increasing length and complexity. It measures the student’s short-term, immediate and working memory, as well as their language comprehension. What is interesting about the administration of this subtest is that the graphic symbols (e.g., objects, shapes, letter and numbers etc.) the student is asked to modify remain covered as the instructions are given (to prevent visual rehearsal). After being presented with the oral instruction the students are expected to move the card covering the stimuli and then to executive the visual-spatial, directional, sequential, and logical if–then the instructions by marking them on the response form. The fact that the visual stimuli remains covered until the last moment increases the demands on the student’s memory and comprehension. The subtest was created to simulate teacher’s use of procedural language (giving directions) in classroom setting (as per developers).
9. The Delayed Story Retelling (DSR) subtest (description above) needs to be administered to the students during the same session as the Story Retelling (SR) subtest, approximately 20 minutes after the SR subtest administration. Despite the relatively short passage of time between both subtests, it is considered to be a measure of long-term memory as related to narrative retelling of reduced complexity. Here, the examiner can compare student’s performance to determine whether the student did better or worse on either of these measures (e.g., recalled more information after a period of time passed vs. immediately after being read the story). However, as mentioned previously, some students may recall this previously presented story fairly accurately and as a result may obtain an average score despite a history of teacher/parent reported long-term memory limitations. Consequently, it may be important for the examiner to supplement the administration of this subtest with a recall of a movie/book recently seen/read by the student (a few days ago) in order to compare both performances and note any weaknesses/limitations.
10. The Nonword Reading (NR) subtest (description above) requires students to decode nonsense words of increasing length and complexity. What I love about this subtest is that the students are unable to effectively guess words (as many tend to routinely do when presented with real words). Consequently, the presentation of this subtest will tease out which students have good letter/sound correspondence abilities as well as solid orthographic, morphological and phonological awareness skills and which ones only memorized sight words and are now having difficulty decoding unfamiliar words as a result. 
11. The Reading Fluency (RF) subtest (description above) requires students to efficiently read facts which make up simple stories fluently and correctly. Here are the key to attaining an average score is accuracy and automaticity. In contrast to the previous subtest, the words are now presented in meaningful simple syntactic contexts.
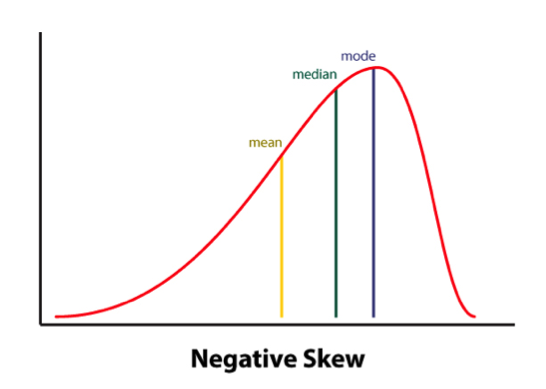
It is important to note that the Reading Fluency subtest of the TILLS has a negatively skewed distribution. As per authors, “a large number of typically developing students do extremely well on this subtest and a much smaller number of students do quite poorly.”
Thus, “the mean is to the left of the mode” (see publisher’s image below). This is why a student could earn an average standard score (near the mean) and a low percentile rank when true percentiles are used rather than NCE percentiles (Normal Curve Equivalent). 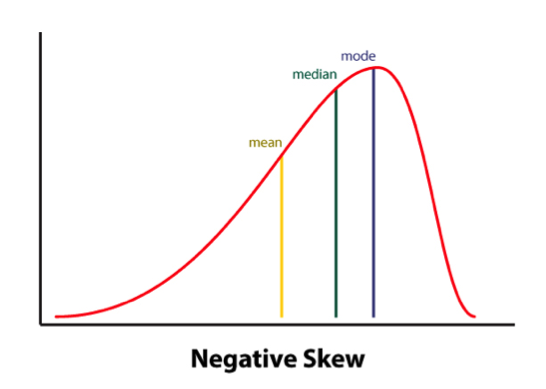
Consequently under certain conditions (See HERE) the percentile rank (vs. the NCE percentile) will be a more accurate representation of the student’s ability on this subtest.
Indeed, due to the reduced complexity of the presented words some students (especially younger elementary aged) may obtain average scores and still present with serious reading fluency deficits.
I frequently see that in students with average IQ and go to long-term memory, who by second and third grades have managed to memorize an admirable number of sight words due to which their deficits in the areas of reading appeared to be minimized. Recommendation: If you suspect that your student belongs to the above category I highly recommend supplementing this subtest with an informal measure of reading fluency. This can be done by presenting to the student a grade level text (I find science and social studies texts particularly useful for this purpose) and asking them to read several paragraphs from it (see HERE and/or HERE).
As the students are reading I calculate their reading fluency by counting the number of words they read per minute. I find it very useful as it allows me to better understand their reading profile (e.g, fast/inaccurate reader, slow/inaccurate reader, slow accurate reader, fast/accurate reader). As the student is reading I note their pauses, misreadings, word-attack skills and the like. Then, I write a summary comparing the students reading fluency on both standardized and informal assessment measures in order to document students strengths and limitations.
12. The Written Expression (WE) subtest (description above) needs to be administered to the students immediately after the administration of the Reading Fluency (RF) subtest because the student is expected to integrate a series of facts presented in the RF subtest into their writing sample. There are 4 stories in total for the 4 different age groups.
The examiner needs to show the student a different story which integrates simple facts into a coherent narrative. After the examiner reads that simple story to the students s/he is expected to tell the students that the story is okay, but “sounds kind of “choppy.” They then need to show the student an example of how they could put the facts together in a way that sounds more interesting and less choppy by combining sentences (see below). Finally, the examiner will ask the students to rewrite the story presented to them in a similar manner (e.g, “less choppy and more interesting.”)

After the student finishes his/her story, the examiner will �analyze it and generate the following scores: a discourse score, a sentence score, and a word score. Detailed instructions as well as the Examiner’s Practice Workbook are provided to assist with scoring as it takes a bit of training as well as trial and error to complete it, especially if the examiners are not familiar with certain procedures (e.g., calculating T-units).
Full disclosure: Because the above subtest is still essentially sentence combining, I have only used this subtest a handful of times with my students. Typically when I’ve used it in the past, most of my students fell in two categories: those who failed it completely by either copying text word for word, failing to generate any written output etc. or those who passed it with flying colors but still presented with notable written output deficits. Consequently, I’ve replaced Written Expression subtest administration with the administration of written standardized tests, which I supplement with an informal grade level expository, persuasive, or narrative writing samples.
Having said that many clinicians may not have the access to other standardized written assessments, or lack the time to administer entire standardized written measures (which may frequently take between 60 to 90 minutes of administration time). Consequently, in the absence of other standardized writing assessments, this subtest can be effectively used to gauge the student’s basic writing abilities, and if needed effectively supplemented by informal writing measures (mentioned above).
13. The Social Communication (SC) subtest (description above) assesses the students’ ability to understand vocabulary associated with communicative intentions in social situations. It requires students to comprehend how people with certain characteristics might respond in social situations by formulating responses which fit the social contexts of those situations. Essentially students become actors who need to act out particular scenes while viewing select words presented to them.
Full disclosure: Similar to my infrequent administration of the Written Expression subtest, I have also administered this subtest very infrequently to students. Here is why.
I am an SLP who works full-time in a psychiatric hospital with children diagnosed with significant psychiatric impairments and concomitant language and literacy deficits. As a result, a significant portion of my job involves comprehensive social communication assessments to catalog my students’ significant deficits in this area. Yet, past administration of this subtest showed me that number of my students can pass this subtest quite easily despite presenting with notable and easily evidenced social communication deficits. Consequently, I prefer the administration of comprehensive social communication testing when working with children in my hospital based program or in my private practice, where I perform independent comprehensive evaluations of language and literacy (IEEs).
Again, as I’ve previously mentioned many clinicians may not have the access to other standardized social communication assessments, or lack the time to administer entire standardized written measures. Consequently, in the absence of other social communication assessments, this subtest can be used to get a baseline of the student’s basic social communication abilities, and then be supplemented with informal social communication measures such as the Informal Social Thinking Dynamic Assessment Protocol (ISTDAP) or observational social pragmatic checklists.
14. The Digit Span Forward (DSF) subtest (description above) is a relatively isolated measure of short term and verbal working memory ( it minimizes demands on other aspects of language such as syntax or vocabulary).
15. The Digit Span Backward (DSB) subtest (description above) assesses the student’s working memory and requires the student to mentally manipulate the presented stimuli in reverse order. It allows examiner to observe the strategies (e.g. verbal rehearsal, visual imagery, etc.) the students are using to aid themselves in the process. Please note that the Digit Span Forward subtest must be administered immediately before the administration of this subtest.
SLPs who have used tests such as the Clinical Evaluation of Language Fundamentals – 5 (CELF-5) or the Test of Auditory Processing Skills – Third Edition (TAPS-3) should be highly familiar with both subtests as they are fairly standard measures of certain aspects of memory across the board.
To continue, in addition to the presence of subtests which assess the students literacy abilities, the TILLS also possesses a number of interesting features.
For starters, the TILLS Easy Score, which allows the examiners to use their scoring online. It is incredibly easy and effective. After clicking on the link and filling out the preliminary demographic information, all the examiner needs to do is to plug in this subtest raw scores, the system does the rest. After the raw scores are plugged in, the system will generate a PDF document with all the data which includes (but is not limited to) standard scores, percentile ranks, as well as a variety of composite and core scores. The examiner can then save the PDF on their device (laptop, PC, tablet etc.) for further analysis.
The there is the quadrant model. According to the TILLS sampler (HERE) “it allows the examiners to assess and compare students’ language-literacy skills at the sound/word level and the sentence/ discourse level across the four oral and written modalities—listening, speaking, reading, and writing” and then create “meaningful pro�files of oral and written language skills that will help you understand the strengths and needs of individual students and communicate about them in a meaningful way with teachers, parents, and students. (pg. 21)”

Then there is the Student Language Scale (SLS) which is a one page checklist parents, teachers (and even students) can fill out to informally identify language and literacy based strengths and weaknesses. It allows for meaningful input from multiple sources regarding the students performance (as per IDEA 2004) and can be used not just with TILLS but with other tests or in even isolation (as per developers).
Furthermore according to the developers, because the normative sample included several special needs populations, the TILLS can be used with students diagnosed with ASD, deaf or hard of hearing (see caveat), as well as intellectual disabilities (as long as they are functioning age 6 and above developmentally).
According to the developers the TILLS is aligned with Common Core Standards and can be administered as frequently as two times a year for progress monitoring (min of 6 mos post 1st administration).
With respect to bilingualism examiners can use it with caution with simultaneous English learners but not with sequential English learners (see further explanations HERE). Translations of TILLS are definitely not allowed as they will undermine test validity and reliability.
So there you have it these are just some of my very few impressions regarding this test. Now to some of you may notice that I spend a significant amount of time pointing out some of the tests limitations. However, it is very important to note that we have research that indicates that there is no such thing as a “perfect standardized test” (see HERE for more information). All standardized tests have their limitations.
Having said that, I think that TILLS is a PHENOMENAL addition to the standardized testing market, as it TRULY appears to assess not just language but also literacy abilities of the students on our caseloads.
That’s all from me; however, before signing off I’d like to provide you with more resources and information, which can be reviewed in reference to TILLS. For starters, take a look at Brookes Publishing TILLS resources. These include (but are not limited to) TILLS FAQ, TILLS Easy-Score, TILLS Correction Document, as well as 3 FREE TILLS Webinars. There’s also a Facebook Page dedicated exclusively to TILLS updates (HERE).
But that’s not all. Dr. Nelson and her colleagues have been tirelessly lecturing about the TILLS for a number of years, and many of their past lectures and presentations are available on the ASHA website as well as on the web (e.g., HERE, HERE, HERE, etc). Take a look at them as they contain far more in-depth information regarding the development and implementation of this groundbreaking assessment.
To access TILLS fully-editable template, click HERE
Disclaimer: I did not receive a complimentary copy of this assessment for review nor have I received any encouragement or compensation from either Brookes Publishing or any of the TILLS developers to write it. All images of this test are direct property of Brookes Publishing (when clicked on all the images direct the user to the Brookes Publishing website) and were used in this post for illustrative purposes only.
References:
Leclercq A, Maillart C, Majerus S. (2013) Nonword repetition problems in children with SLI: A deficit in accessing long-term linguistic representations? Topics in Language Disorders. 33 (3) 238-254.
Related Posts:
 In today’s guest post, Natalie Romanchukevich advises readers on how to create opportunities to expand children’s spontaneous communication skills.
In today’s guest post, Natalie Romanchukevich advises readers on how to create opportunities to expand children’s spontaneous communication skills.






















 Recently I’ve purchased the Executive Functions Test-Elementary (EFT-E) by Linguisystems and used it with a few clients in my private practice and outpatient hospital-based school program
Recently I’ve purchased the Executive Functions Test-Elementary (EFT-E) by Linguisystems and used it with a few clients in my private practice and outpatient hospital-based school program Three years ago I wrote a blog post entitled: “
Three years ago I wrote a blog post entitled: “